Implementing New CMS Translation Requirements for CY 2024 – UPDATED*
By Elizabeth Lippincott, Katarina Weessies and Liz Hughes
On April 12, 2023, the Centers for Medicare & Medicaid Services (CMS) published a final rule revising translation and accessibility requirements for Medicare Advantage and Part D materials. The final rule includes expanded availability of translated and accessible materials.
Before the final rule became effective, Medicare plans were already subject to translation and accessibility standards for required materials. For example, the previous rule required plans to provide materials for any non-English language of at least 5 percent of individuals in service area. However, the previous rule did not clarify whether translated materials needed to be available on a standing basis or if the services should only be provided upon request. The previous rule also required that plans provide auxiliary aids and services, including interpreters and alternate formats, for accessibility purposes, as well as a multi-language insert explaining that translation services are available.
New Requirements and Clarifications
The final rule requires plans to provide translated versions of required materials on a standing basis in languages spoken by at least 5 percent of individuals in a plan’s service area.
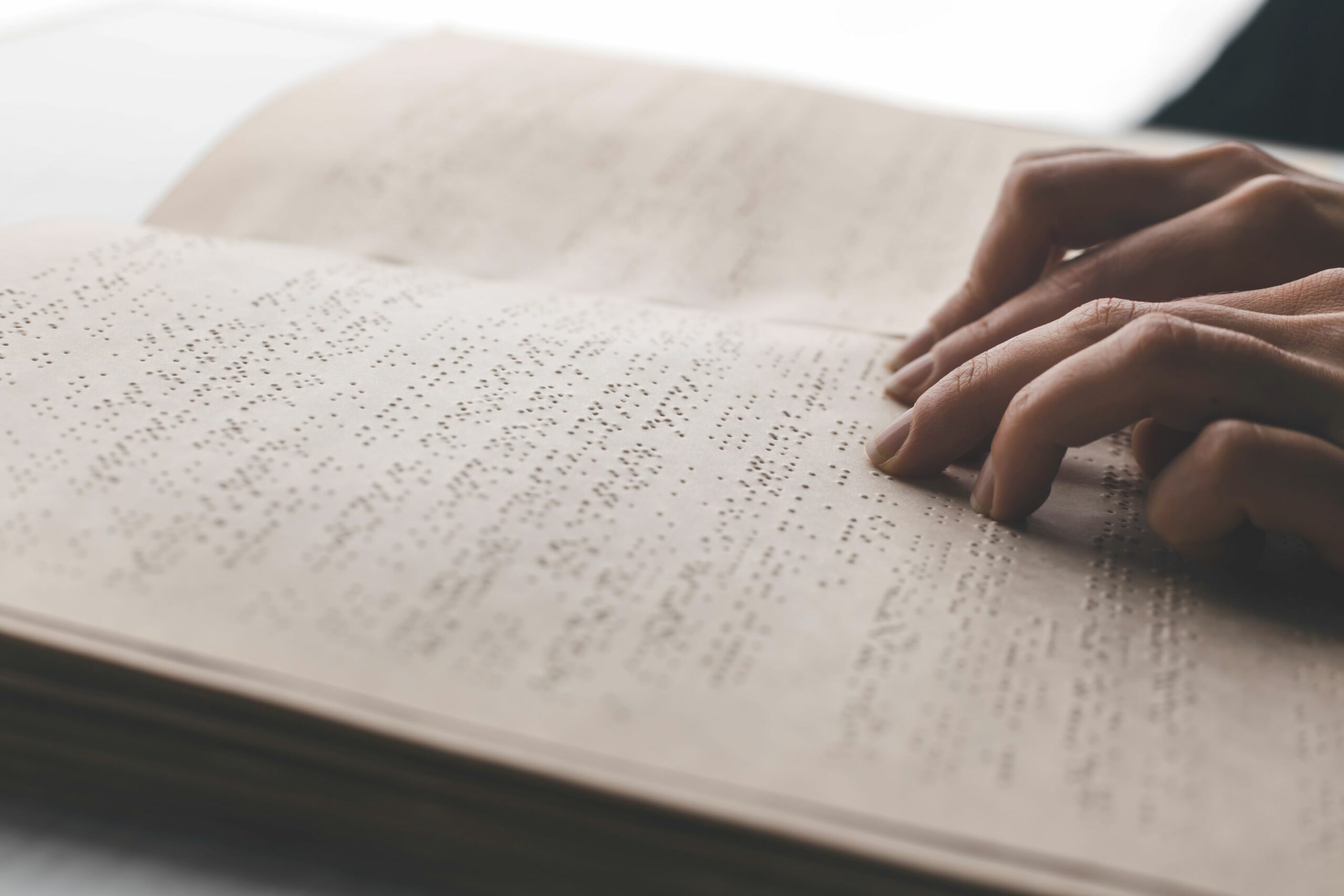
Plans must also provide materials in an accessible format, such as braille or large print, upon request. When an individual requests translated materials, every required material should be provided in the requested manner (alternate language and/or format) on a standing basis, meaning for as long as the individual is enrolled or until the enrollee requests the materials in a different manner. The rule clarifies that certain SNPs must translate materials based on both the new MA standards and any applicable Medicaid standards.
Implementation Issues
The Preamble instructed plans on addressing implementation when an enrollee makes a request that may be difficult to fulfill within a required timeframe:
“If there are certain facts and circumstances when the plan has difficulty producing an alternate format within the applicable adjudication timeframe, the plan should first work proactively with the individual to achieve equivalent communications, but nevertheless document the facts and circumstances, including an explanation of why the documentation could not be produced within the regulatory timeframe, and make best efforts to communicate the information to the individual via the most effective means.”
Reg. 22224, 22228 (April 12, 2023).
The rule leaves some flexibility to determine which materials the enrollee truly wants to receive in the alternate format. For example, an individual might wish to receive a paper EOB in an alternate format (e.g. Braille) but would prefer to speak with customer service representatives by phone to search for providers in a directory, as opposed to receiving a paper version. In implementing the requirement, plans may want to ask which materials and notices the enrollee would like to receive in the alternate format, and it would be appropriate to mention for the enrollee how voluminous some materials might be in paper alternate formats.
Plans may want to consider having an internal task force of representatives trained to help members obtain the information they need in the most useful manner to meet the enrollees’ needs for information without inconveniencing them or wasting resources. The Preamble recommends clarifying enrollee wishes, adding that plans should reach out to confirm the enrollee’s need for specific materials in translated or accessible form.
It is also important to note that plans can learn of, and must respond to, an enrollee’s need for translated or accessible materials without the enrollee making a request for the materials directly. The enrollee’s need can also come up during a health risk assessment or another touch point. The plan must provide required materials in the translated or accessible format regardless of how the plan learned of the need, though the rule leaves room for plan representatives to contact enrollees to clarify their wishes for communication formats.
To best administer translation services, plans should have a system in plan to document all communications with enrollees around translation and alternate formats and to track enrollee requests for materials in translated or accessible form. Plans may already have a similar system, since this particular portion of the rule is consistent with requirements for fulfilling requests for hard copy materials under previous rules. Under certain circumstances, plans are also permitted to extend timeframes for providing materials.
Written Non-English Translation for Languages under 5 Percent Threshold
The final rule contains some ambiguity around what a plan’s obligation is when an enrollee who speaks a non-English language, that does not meet the 5 percent threshold in the service area, requests translated written materials. A number of passages in the rule’s preamble discuss written translation requirements without reference to the 5 percent threshold, suggesting that the requirement applies to all requests for non-English translations. For example:
“We believe that it is a substantial burden for enrollees to have to request each material in a non-English language or accessible format and that requiring enrollees to do so could impede access to care. It is also possible that enrollees may require materials in both an alternate format and a non-English language (for example Spanish braille). In addition, to ensure the ICPs are developed in consultation with the enrollee as required at § 422.101(f)(1)(ii), it is important that ICP materials be provided in the enrollee’s primary language and, where appropriate, in an accessible format. As described at 87 FR 79522 of the proposed rule, research has found patients with limited English proficiency experience negative health outcomes due to the barriers they encounter, including when interacting with their doctors and care team members. . .
We believe that there are many ways for MA organizations and Part D sponsors to learn of an enrollee’s need for an accessible format and language needs and maintain this information.”
88 Fed. Reg. at 22225 (April 12, 2023).
Looking at the revised text of the regulation itself (42 CFR 422.2267(a)) in context, however, the requirement to translate written materials into non-English languages is limited by the 5 percent threshold:
(a) Standards for required materials and content. All required materials and content, regardless of categorization as standardized in paragraph (b) of this section or model in paragraph (c) of this section, must meet the following:
(1) Be in a 12pt font, Times New Roman or equivalent.
(2) For markets with a significant non-English speaking population, be in the language of these individuals. Specifically, MA organizations must translate required materials into any non-English language that is the primary language of at least 5 percent of the individuals in a plan benefit package (PBP) service area.
(3) Be provided to enrollees on a standing basis in any non-English language identified in paragraphs (a)(2) and (4) of this section or accessible format upon receiving a request for the materials in a non-English language or accessible format or when otherwise learning of the enrollee’s primary language or need for an accessible format. This requirement also applies to the individualized plans of care described in § 422.101(f)(1)(ii) for special needs plan enrollees.
(4) For any fully integrated dual eligible special needs plan or highly integrated dual eligible special needs plan, as defined at § 422.2, or applicable integrated plan, as defined at § 422.561, be translated into the language(s) required by the Medicaid translation standard as specified through their capitated Medicaid managed care contract in addition to the language(s) required by the Medicare translation standard in paragraph (a)(2) of this section.
(5) Be provided to the beneficiary within CMS’s specified timeframes.
42 CFR 422.2267(a) (emphasis added).
The new requirement for written materials to be provided on a “standing basis” in subsection (a)(3) sits within the regulatory requirement of written translation of materials in languages spoken by at least 5 percent of individuals in the plan benefit package’s service area, in subsections (a)(2) and (4). In section b of the cost summary table on page 22124 of the Preamble to the final rule, CMS describes the translation requirements as limited by the 5 percent threshold: “We are finalizing requirements that: (1) MA organizations, cost plans, and Part D sponsors provide materials to enrollees on a standing basis in any non-English languages [sic] that is the primary language of at least 5 percent of the individuals in that service area and/or accessible formats.”
CMS’ expectations for requested written translations, as applied to languages below the 5 percent threshold, could be clearer. At this time, however, we read the requirement of written translations as limited to languages meeting the 5 percent threshold.
These regulations became effective June 5, 2023.
*6/26/23 – Updated to reflect our evolving interpretation of the final rule as it applies to translation of written materials into non-English languages spoken by less than 5 percent of a service area population. Please note that this briefing is for informational purposes and does not constitute legal advice.




