Healthcare History – In the Beginning
By Elizabeth B. Lippincott
“The past is never dead. It’s not even past.” William Faulkner
As a health plan lawyer for over two decades, I have seen the intricacies—and curiosities—of our healthcare financing and regulatory system up close. Before I studied political science, law, and theology, I learned from my history teacher father that knowledge of the past is critical to making sense the present. My dad taught me to try to place what I observe in historical perspective to understand it better.
The United States’ healthcare financing and regulatory system is more than complicated. It’s Byzantine. It reminds me of a house that was built room-by-room by different people over the course of many decades, with no over-arching design or plan. Our incrementally constructed, public-private hodge-podge of health coverage, with its wide array of state and federal programs, agencies, and rules, begs the question: Who came up with this? How did we get here?
The aim of this Healthcare History series of articles is to answer those questions. To kick off this series, we will start from the beginning, with an overview of the three branches of the United States government, what this structure was designed to do—and what it was designed to prevent. This background is key to understanding the otherwise inexplicable morass of health law in the U.S.
The U.S. Constitution was adopted in 1789, but our story starts before that with its precursor, the Articles of Confederation, which were ratified during the Revolutionary War. The Articles of Confederation reserved almost all powers to the sovereign states, with a single chamber legislature for the Confederation, in which each state had equal representation regardless of population. This first congress had very limited authority to make treaties, maintain armed forces, operate a postal service, and coin money, and it lacked the power to levy taxes, raise troops, or regulate interstate commerce. The executive and judicial branches did not exist. The president merely presided over the legislature.
The framers of the U.S. Constitution sought to address a perceived need for expanded federal government functions while assuaging the former colonists’ deeply held wariness of unlimited government power. To that end, the framers implemented the system of checks and balances between the three branches of government that is at the core of our democracy, and which they designed to make it difficult for the federal government to take sweeping action. Under the new Constitution, the federal government had broader powers than the previous Confederation, including the right to impose taxes, raise a military, and regulate interstate commerce. However, these expanded powers were distributed across three co-equal branches of government: 1) two chambers of Congress, the House of Representatives and the Senate; 2) an executive branch headed by the President, who may be from a different political party than the majority of either chamber of Congress, with veto power over legislation; and 3) a federal judiciary to address, among other things, disputes between the states. With this separation of powers, the framers prioritized protection against abrupt or oppressive government action over the efficiencies associated with more centralized control.
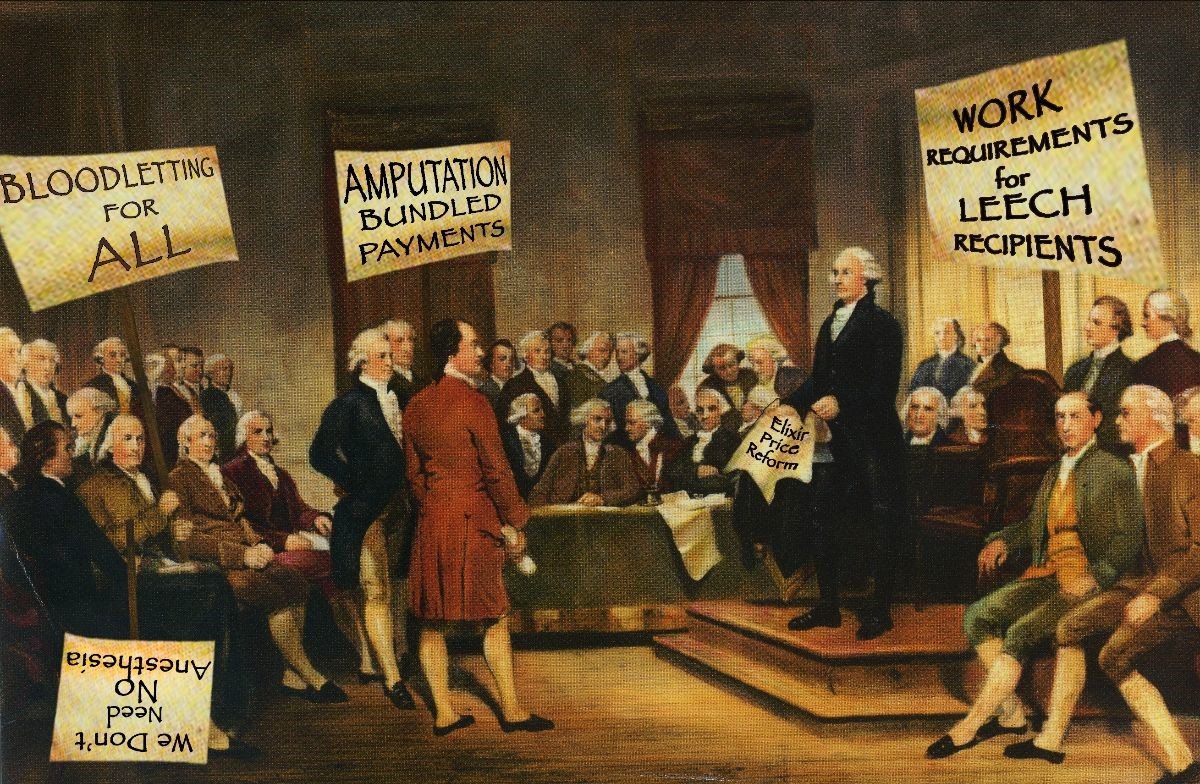
In 1789, the framers almost certainly could not have imagined healthcare—at least not as it exists today—as one of the issues this new federal government, with its broadly distributed powers, would need to address. The healthcare available at the time was limited, privately funded, and often ineffective. At the time of the American Revolution, there were around 3,500 medical practitioners in America, an estimated 400 of whom had formal training, and just a handful of hospitals. Life expectancy averaged around age 34 for men and 36 for women, though because of the prevalence of childhood illness and death, after reaching age 20, a man could expect to live to the ripe old age of 54 and a woman to 56. At a time when a physician might have accepted a ham or basket of vegetables from a patient as compensation for services, no one would have predicted that hospitals would someday submit electronic claims to managed care organizations to be reimbursed with federal funds.
Commentators today often compare healthcare in the United States to other western democracies, such as Canada and the United Kingdom. Notably, those two countries have parliamentary systems of government, with a Prime Minister from the same political party that holds a majority of seats in parliament, as well as an elected House of Commons that functions as the primary legislative chamber, in contrast to the U.S. system in which the President can be from a different party from the majority in one or both chambers of Congress, and in which the House and the Senate are equally active and powerful bodies in the development and passage of legislation. The composition of the U.S. Senate enhances the representative influence of voters in less populous states, and the filibuster creates an additional hurdle to the passage of legislation without super-majority support in the Senate. In contrast, parliamentary systems, with relatively streamlined legislative pathways, reflect different priorities and impose fewer checks and balances on government action, which helps to explain, in part, why the healthcare system in the United States differs from its counterparts in some other countries.
Imagine for a moment if the U.S. House of Representatives functioned as our primary lawmaking body, and instead of a President, we had a Prime Minister from the House’s ruling party. Our healthcare system might look a lot different. That some parliamentary systems have generated more centralized healthcare financing systems should come as no surprise, and neither should the incremental and sometimes disjointed patchwork of programs that has evolved in the United States. The very structure of our system of government makes anything other than incremental policy change difficult to accomplish.
The next Healthcare History installment will address one of the most consequential accidents of history in U.S. healthcare: employer-based health insurance.
© 2021 Strategic Health Law




